Kidney Transplant

A kidney transplant is a surgery to place a healthy kidney from a living or deceased donor into a person whose kidneys no longer function properly.
The kidneys are two bean-shaped organs located on each side of the spine just below the rib cage. Each is about the size of a fist. Their main function is to filter and remove waste, minerals and fluid from the blood by producing urine.
When kidneys lose this filtering ability, harmful levels of fluid and waste accumulate in the body, which can raise blood pressure and result in kidney failure (end-stage renal disease). End-stage renal disease occurs when the kidneys have lost about 90% of their ability to function normally.
Common causes of end-stage kidney disease include:
- Diabetes
- Chronic, uncontrolled high blood pressure
- Chronic glomerulonephritis — an inflammation and eventual scarring of the tiny filters within the kidneys
- Polycystic kidney disease
People with end-stage renal disease need to have waste removed from their bloodstream via a machine (dialysis) or a kidney transplant to stay alive.
At Medical Associates Hospital, health care professionals trained in many medical specialties work together as a team to ensure favorable outcomes from your kidney transplant.
Having all of this subspecialized expertise in a single place, focused on you, means that you’re not just getting one opinion — your care is discussed among the team, your test results are available quickly, appointments are scheduled in coordination, and your transplant care team works together to determine what’s best for you.
Types of Kidney Transplant
Deceased – donor Kidney Transplant
- A deceased donor kidney transplant is a surgery to give you a healthy kidney from someone who has just died. The person may have died in an accident or been recently removed from life support in a hospital.
Living – donor Kidney Transplant
- A living donor is someone who has agreed to donate their kidney to you while they are still alive. This is possible as nearly everyone has two kidneys, but can lead normal healthy lives with just one kidney. A living donor will need an operation to remove one of their kidneys so it can be transplanted into you.
Pre-emptive Kidney Transplant
- If you have kidney disease, getting a transplant before you need to start dialysis is called a preemptive transplant. Getting a transplant not long after kidneys fail (but with some time on dialysis) is referred to as an early transplant.
Why is it done?
A kidney transplant is often the treatment of choice for kidney failure, compared with a lifetime on dialysis. A kidney transplant can treat chronic kidney disease or end-stage renal disease to help you feel better and live longer.
Compared with dialysis, kidney transplant is associated with:
- Better quality of life
- Lower risk of death
- Fewer dietary restrictions
- Lower treatment cost
Some people may also benefit from receiving a kidney transplant before needing to go on dialysis, a procedure known as preemptive kidney transplant.
But for certain people with kidney failure, a kidney transplant may be riskier than dialysis. Conditions that may prevent you from being eligible for a kidney transplant include:
- Advanced age
- Severe heart disease
- Active or recently treated cancer
- Dementia or poorly controlled mental illness
- Alcohol or drug abuse
- Any other factor that could affect the ability to safely undergo the procedure and take the medications needed after a transplant to prevent organ rejection
Only one donated kidney is needed to replace two failed kidneys, making living-donor kidney transplantation an option.
If a compatible living donor isn’t available, your name may be placed on a kidney transplant waiting list to receive a kidney from a deceased donor.
How long you have to wait for a deceased donor organ depends on the degree of matching or compatibility between you and the donor, time on dialysis and on the transplant waitlist, and expected survival post-transplant. Some people get a match within several months, and others may wait several years.
What are your risks?
Kidney transplantation can treat advanced kidney disease and kidney failure, but the surgery isn’t a cure. Some forms of kidney disease may return after a transplant.
The health risks associated with a kidney transplant include those associated directly with the surgery and rejection of the donor organ. Risks also include the side effects of taking anti-rejection medications (immunosuppressants) needed to prevent the body from rejecting the donated kidney.
Deciding whether a kidney transplant is right for you is a personal decision that deserves careful thought and consideration of the serious risks and benefits. Talk through your decision with your family, friends and other trusted advisers.
Complications of the Procedure
Anti-rejection Medication Side Effects
Kidney transplant surgery carries a risk of significant complications, including:
- Blood clots and bleeding
- Leaking from or blockage of the tube that links the kidney to the bladder (ureter)
- Infection
- Failure or rejection of the donated kidney
- An infection or cancer that can be passed on from the donated kidney
- Death, heart attack and stroke
After a kidney transplant, you’ll take medications to help prevent your body from rejecting the donor kidney. These medications can cause a variety of side effects, including:
- Bone thinning and bone damage
- Diabetes
- Excessive hair growth or hair loss
- High blood pressure
- High cholesterol
Other side effects may include:
- Increased risk of cancer, particularly skin cancer and lymphoma
- Infection
- Puffiness
- Weight gain
- Acne
What to Expect
Before the Procedure
Finding a match
A kidney donor can be living or deceased, related or unrelated to you. Your transplant team will consider several factors when evaluating whether a donor kidney will be a good match for you.
Tests to determine whether a donated kidney may be suitable for you include:
Blood typing. It’s preferable to get a kidney from a donor whose blood type matches or is compatible with your own.
Transplants involving a donor and recipient with incompatible blood types are also possible but require additional medical treatment before and after transplant to reduce the risk of organ rejection. These are known as ABO incompatible kidney transplants.
- Tissue typing. If your blood type is compatible, the next step is a tissue typing test called human leukocyte antigen (HLA) typing. This test compares genetic markers that increase the likelihood the transplanted kidney will last a long time. A good match means it’s less likely that your body will reject the organ.
Crossmatch. The third and final matching test involves mixing a small sample of your blood with the donor’s blood in the lab. The test determines whether antibodies in your blood will react against specific antigens in the donor’s blood.
A negative crossmatch means they are compatible and your body isn’t as likely to reject the donor kidney. Positive crossmatch kidney transplants also are possible but require additional medical treatment before and after the transplant to reduce the risk of your antibodies reacting to the donor organ.
Additional factors your transplant team may consider in finding the most appropriate donor kidney for you include matching age, kidney size and infection exposure.
Finding a willing living kidney donor is an alternative to waiting for a compatible deceased-donor kidney to become available.
Family members are often the most likely to be compatible living kidney donors. But successful living-donor transplants are also common with kidneys donated from unrelated people, such as friends, co-workers or religious congregation members.
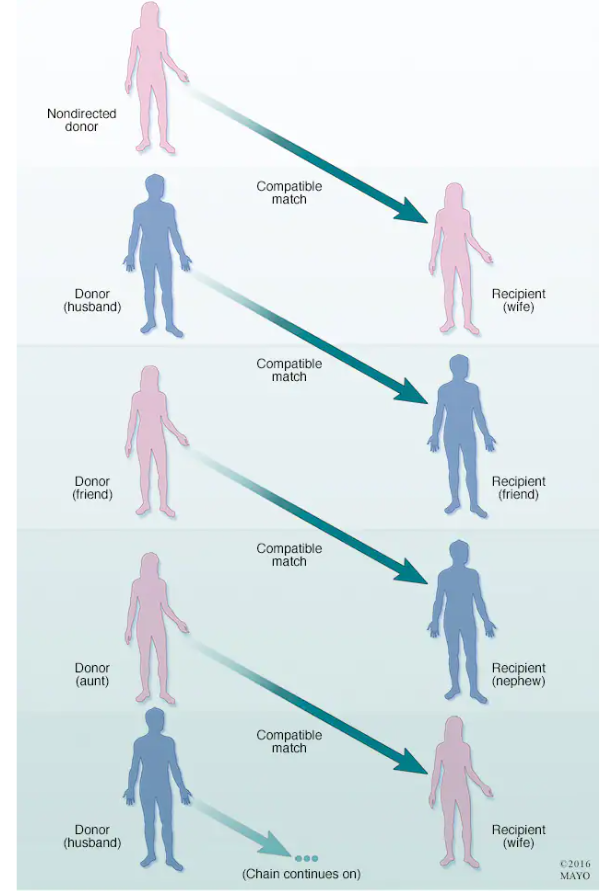
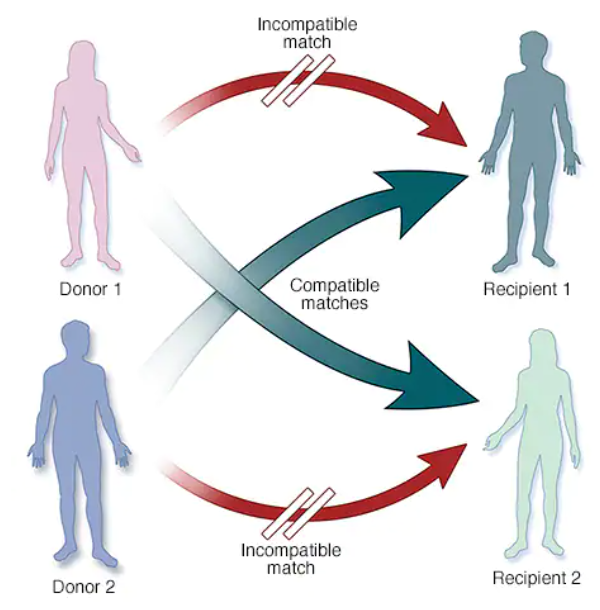
Paired donation is another type of living kidney donation if you have a willing kidney donor whose organ isn’t compatible with you or doesn’t match well for other reasons. Rather than donating a kidney directly to you, your donor may give a kidney to someone who may be a better match. Then you receive a compatible kidney from that recipient’s donor.
In some cases, more than two pairs of donors and recipients may be linked with a living kidney donor who hasn’t named a specific person to receive the kidney. They form a donation chain with several recipients benefiting from the nondirected donor’s gift.
If a compatible living donor isn’t available, your name will be placed on a waiting list for a deceased-donor kidney. Because there are fewer available kidneys than there are people waiting for a transplant, the waiting list continues to grow. The waiting time for a deceased-donor kidney is usually a few years.
Staying Healthy
Whether you’re waiting for a donated kidney or your transplant surgery is already scheduled, work to stay healthy. Being healthy and as active as you’re able can make it more likely you’ll be ready for the transplant surgery when the time comes. It may also help speed your recovery from surgery. Work to:
- Take your medications as prescribed.
- Follow your diet and exercise guidelines.
- Don’t smoke. If you need help quitting, talk to your doctor.
- Keep all appointments with your health care team.
- Stay involved in healthy activities, including relaxing and spending time with family and friends.
Stay in touch with your transplant team and let your team know of any significant changes in your health. If you’re waiting for a donated kidney, make sure the transplant team knows how to reach you at all times. Keep your packed hospital bag ready and make arrangements for transportation to the transplant center.
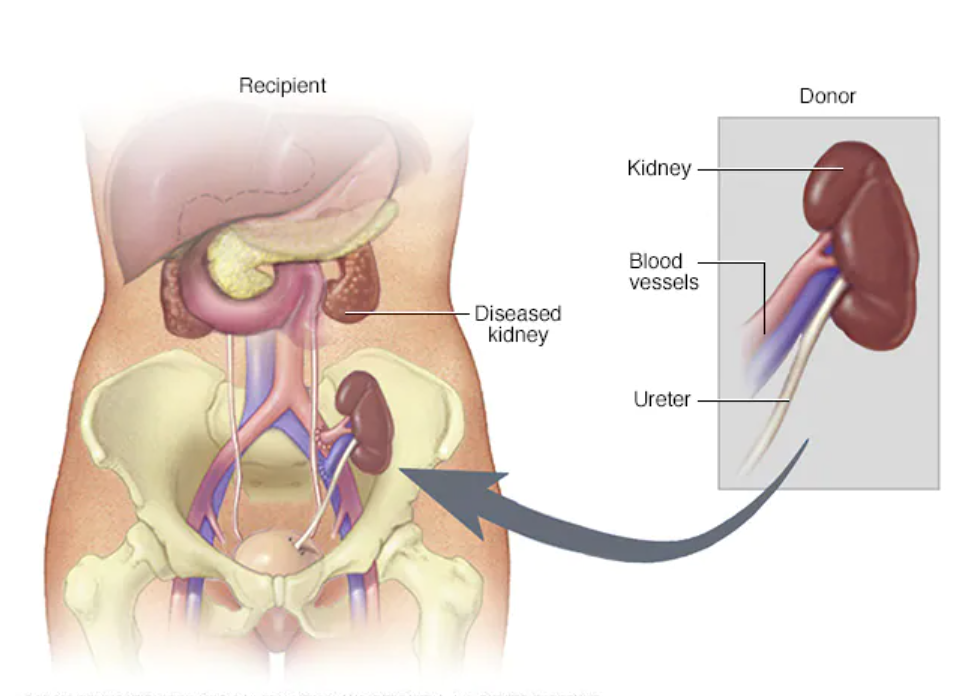
Kidney transplants are performed with general anesthesia, so you’re not awake during the procedure. The surgical team monitors your heart rate, blood pressure and blood oxygen level throughout the procedure.
During the surgery:
- The surgeon makes an incision in the lower part of one side of the abdomen and places the new kidney into the body. Unless your own kidneys are causing complications such as high blood pressure, kidney stones, pain or infection, they are left in place.
- The blood vessels of the new kidney are attached to blood vessels in the lower part of the abdomen, just above one of your legs.
- The new kidney’s ureter — the tube that links the kidney to the bladder — is connected to the bladder.
After the Procedure
After a kidney transplant, you can expect to:
Spend several days to a week in the hospital. Doctors and nurses monitor your condition in the hospital’s transplant recovery area to watch for signs of complications.
Your new kidney will make urine like your own kidneys did when they were healthy. Often this starts immediately. In other people, it may take several days, and you may need temporary dialysis until your new kidneys begin to function properly.
Expect soreness or pain around the incision site while you’re healing. Most kidney transplant recipients can return to work and other normal activities within eight weeks after transplant. Avoid lifting objects weighing more than 10 pounds or exercising other than walking until the wound has healed (usually about six weeks after surgery).
Have frequent checkups as you continue recovering. After you leave the hospital, close monitoring is necessary for a few weeks to check how well your new kidney is working and to make sure your body is not rejecting it.
You may need to have blood tests several times a week and have your medications adjusted in the weeks following your transplant. During this time, if you live in another town, you may need to make arrangements to stay near the transplant center.
- Take medications the rest of your life. You’ll take a number of medications after your kidney transplant. Immunosuppressant drugs help keep your immune system from attacking and rejecting your new kidney. Additional drugs help reduce the risk of other complications, such as infection, after your transplant.
Results
After a successful kidney transplant, your new kidney will filter your blood, and you will no longer need dialysis.
To prevent your body from rejecting your donor kidney, you’ll need medications to suppress your immune system. Because these anti-rejection medications make your body more vulnerable to infection, your doctor may also prescribe antibacterial, antiviral and antifungal medications.
It is important to take all your medicines as your doctor prescribes. Your body may reject your new kidney if you skip your medications even for a short period of time. Contact your transplant team immediately if you are having side effects that prevent you from taking the medications.
After the transplant, be sure to perform skin self-checks and get checkups with a dermatologist to screen for skin cancer. Also, staying up to date with other cancer screening is strongly advised.
Coping and Support
It’s normal to feel anxious or overwhelmed while waiting for a transplant or to have fears about rejection, returning to work or other issues after a transplant. Seeking the support of friends and family members can help you cope during this stressful time.
Your transplant team can also assist you with other useful resources and coping strategies throughout the transplant process, such as:
- Joining a support group for transplant recipients. Talking with others who have shared your experience can ease fears and anxiety.
- Sharing your experiences on social media. Engaging with others who have had a similar experience may help you adjust to your changing situation.
- Finding rehabilitation services. If you’re returning to work, your HR Department may be able to connect you with rehabilitation services locally.
- Setting realistic goals and expectations. Recognize that life after transplant may not be exactly the same as life before transplant. Having realistic expectations about results and recovery time can help reduce stress.
- Educating yourself. Learn as much as you can about your procedure and ask questions about things you don’t understand. Knowledge is empowering.
Diet and Nutrition
After your kidney transplant, you may need to adjust your diet to keep your new kidney healthy and functioning well. You’ll have fewer dietary restrictions than if you were receiving dialysis therapy before your transplant, but you will need to make dietary changes.
Your transplant team includes a nutrition specialist (dietitian) who can discuss your nutrition and diet needs and answer any related questions.
Some of your medications may increase your appetite and make it easier to gain weight. But reaching and maintaining a healthy weight through diet and exercise is just as important for transplant recipients as it is for everyone else to reduce the risk of heart disease, high blood pressure and diabetes.
You may need to keep track of how many calories you consume or limit foods high in sugar and fat.
Your dietitian will also provide you with several healthy food options and ideas to use in your nutrition plan. Your dietitian’s recommendations after kidney transplant may include:
- Eating at least five servings of fruits and vegetables each day
- Avoiding grapefruit and grapefruit juice due to its effect on a group of immunosuppression medications (calcineurin inhibitors)
- Having enough fiber in your daily diet
- Drinking low-fat milk or eating other low-fat dairy products, which is important to maintain optimal calcium and phosphorous levels
- Eating lean meats, poultry and fish
Your dietitian may also recommend:
- Maintaining a low-salt and low-fat diet
- Following food safety guidelines
- Staying hydrated by drinking adequate water and other fluids each day
Exercise
Once you recover from your transplant surgery, exercise and physical activity should be a regular part of your life to continue improving your overall physical and mental health.
After a transplant, regular exercise helps boost energy levels and increase strength. It also helps you maintain a healthy weight, reduce stress, and prevent common post-transplant complications such as high blood pressure and cholesterol levels.
Your transplant team will recommend a physical activity program based on your individual needs and goals.
Soon after your transplant, you should walk as much as you can. Gradually, start incorporating more physical activity into your daily life, including participating in at least 30 minutes of moderate exercise five days a week.
Walking, bicycling, swimming, low-impact strength training and other physical activities you enjoy can all be a part of a healthy, active lifestyle after transplant. But be sure to check in with your transplant team before starting or changing your post-transplant exercise routine.

